There are many different types of headaches, and it is important to be able to determine which type of headache you suffer from in order to properly treat and prevent headaches in the future. In large part, the type of headache is largely dependent on lifestyle, diet and a variety of other factors. While some may suffer from a tension headache that only occurs a couple times each year, others may suffer from migraine or cluster headaches that occur several times each month.
By understanding your lifestyle factors that can increase your risk of developing a headache, along with the different holistic measures that can be taken to prevent different types of headaches, you can prevent a headache from occurring in the first place on many occasions. In the event a headache does still occur, you can fully treat the headache and ensure it does not last for longer than necessary or the symptoms do not worsen.
Each type of headache has its own unique set of symptoms, causes and treatment, and it is important to be able to distinguish between the various types of headaches in order to determine why you are experiencing it in the first place.
Top Related Article: What Causes Migraines And Can They Be Prevented?
In this guide to the different types of headaches, you will learn about the different types of headaches, including signs, symptoms, causes and treatment options for each. The first step to preventing and treating your headaches is to educate yourself on how to do so, and we hope to help you do exactly that.
What Are the Different Types of Headaches?
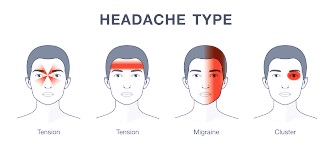
Here are the most common types of headaches people suffer from:
- Tension headaches
- Cluster headaches
- Migraine headaches
- Sinus headaches
- Caffeine headaches
- Exercise headaches
- Head injuries
Of course, there are even more headache types, but the aforementioned seven are the most common. In most cases, those who experience headaches can determine the exact type by examining the specific causes and symptoms of these seven types of headaches.
For each type of headache that is reviewed, you will learn the exact signs and symptoms, causes and treatment options available with each one. Additionally, you will learn how a doctor might diagnose the exact type and severity level of your headache, and we discuss when to see a doctor for each type of headache.
By having a full understanding of each different type of headache, you give yourself a better chance of treating the underlying cause as well as the symptoms before the headache worsens, and you will know when it is necessary to seek professional help in the event the headaches become chronic or individual episodes of a headache become too severe.
Many headaches can be properly and appropriately dealt with at home with holistic treatment options, although more severe headaches, or headaches that become very constant, may require professional treatment.
Without further ado, let’s get into reviewing the signs and symptoms, causes and treatment options for each of the seven most common headache types.
1. Tension Headaches


Most tension headaches are fairly mild and not overly serious, although the severity and frequency one experiences tension headaches may vary, with the most severe cases of tension headaches occurring several times a week which can drastically affect one’s ability to carry out their daily routine.
Fortunately, tension headaches are highly treatable and can oftentimes be prevented when the right lifestyle and medical measures are taken.
Signs and symptoms
There are three main symptoms that are most commonly associated with tension headaches, which are:
- Throbbing head pain
- Pressure surrounding the forehead
- Tenderness around the forehead
The most identifiable symptom of a tension headache is a dull, throbbing pain in the forehead and scalp regions. Usually there is a lot of pressure that comes along with a tension headache, which as mentioned earlier can feel as if a tight band is wrapped around your head. Also, there is oftentimes some tenderness and sensitivity to the forehead area.
On severe occasions, tension headaches can also show migraine-like symptoms, such as sensitivity to light or sensitivity to loud noises. However, most instances of a tension headache are fairly mild and do not last for more than several hours when proper treatment is administered.
Many often confuse a tension headache with a migraine, although a migraine is typically more severe and has distinguishable symptoms that are not present with a tension headache (see below).
Causes
Perhaps the best way to determine whether a headache is a tension headache or a more serious concern such as a migraine is to look at the most probable cause, rather than the signs and symptoms.
Here are the most common causes of a tension headache:
- Severe fatigue
- Emotional stress
- Cold temperatures
- Eye strain
Perhaps the main cause of tension headaches is severe fatigue, which typically is brought on by constant focus on an activity without taking proper breaks or receiving an adequate amount of rest. Subsequently, those who work in an office – especially those vulnerable to eye strain – are at greater risk of developing a tension headache.
Also, exposure to very hot or cold temperatures is believed to lead to tension headaches. Those who are emotionally stressed are also at greater risk of developing a tension headache, and it is important to minimize stress in order to prevent a tension headache from developing.
Diagnosis
In many cases – especially in instances when the individual experiences chronic tension headaches – it is important to visit a doctor in order to determine whether or not the type of headache is a tension headache or something else.
When visiting a doctor, the doctor is likely to conduct an examination, which includes documenting the patient’s symptoms and medical history. They may also run various tests to try and determine the exact type of headache, which may include CT scans and x-rays.
In most cases, tension headaches can be diagnosed by reviewing the patient’s lifestyle and medical history as well as their current symptoms, without the need for additional testing.
Treatment
In many instances tension headaches can be treated with holistic care at home. The best way to treat tension headaches is to simply receive an adequate amount of rest, especially if the tension headache is caused by fatigue or emotional stress.
Since rest can be difficult when suffering from the symptoms of a tension headache, it is helpful to wear an eye mask in order to rest the eyes and head properly.
Also, there are certain over-the-counter medications that are helpful for treating the symptoms of the tension headache, such as Bayer or Excedrin, which are specifically designed for headache relief. In more severe instances, a prescription strength pain reliever may be in order to effectively treat the symptoms.
While professional care is sometimes necessary for tension headaches, the best way to treat tension headaches is to treat the underlying cause, which is generally the result of lifestyle choices, such as working long hours working without adequate breaks or emotional stress.
Top Related Article: How to Achieve Migraine Relief
When to see a doctor
Oftentimes even the worst cases of tension headaches do not pose any great health risk, and the most severe symptom one is likely to experience is sensitivity to light or sound. However, tension headaches can cause those who suffer from them to drastically alter their lifestyle, especially if they become chronic.
Therefore, anytime tension headaches begin to occur on a consistent basis, it is important to see a doctor in order to find a long-term treatment and prevention plan for the tension headaches.
Also, tension headaches that become extremely severe to the point where they are close to intolerable should be treated by a doctor as there is a high likelihood that the type of headache is not a tension headache, but rather a migraine or other form of severe head pain.
2. Cluster Headaches


There are two different types of cluster headaches, which are chronic and episodic. Chronic cluster headaches are headaches that occur consistently for more than a year and then followed by a brief moment of being headache-free. Episodic cluster headaches may occur frequently for several months or less, and then the patient becomes headache-free for a similar length of time before the headaches start back.
Signs and symptoms
In many ways the signs and symptoms of a cluster headache are similar to a tension headache, but there are certain signs that can help individuals distinguish a cluster headache from a tension headache, including the following:
- A sudden onset of symptoms
- More severe pain
- Pain that lasts for several hours
- Pressure on one side of the head
Whereas a tension headache can cause a mild level of pain that progressively worsens, cluster headaches often have a sudden onset and can seemingly occur out of nowhere. The pain with cluster headaches is typically much worse than a tension headache, and the worst of the pain is usually in the first several hours after symptoms present themselves.
In many instances cluster headaches go away after several hours, and it is far rarer for cluster headaches to linger than it is with tension headaches. Lastly, cluster headaches most often affect one side of the head much more than the other.
Related Article: Eye Strain Treatment
Causes
The exact cause of cluster headaches is still uncertain, although cluster headaches are believed to stem from the dilation of blood vessels. When blood vessels near the brain are dilated – meaning they widen or swell – they place pressure on the trigeminal nerve, which is responsible for transmitting sensations from the face to the brain.
While knowing the science behind why cluster headaches occur helps with treatment, it is still a mystery as to why the dilation occurs in the first place, which makes prevention slightly more complicated.
However, there are certain individuals more at risk than others when it comes to cluster headaches. Cluster headaches most commonly occur in individuals between adolescence and middle age. Also, certain drugs such as alcohol and cocaine are believed to put individuals at greater risk of suffering from cluster headaches.
Diagnosis
In the event cluster headaches occur, it is very important to visit a doctor to ensure the condition is not a more serious medical concern, such as a brain tumor.
The doctor is likely to utilize various diagnostic measures to determine whether or not the headaches are a result of cluster headaches or another type of headache or medical condition.
Most diagnostic procedures for cluster headaches involve a complete analysis of the patient’s medical history, including their daily lifestyle and previous medical treatment. The doctor is also likely to conduct a thorough physical examination and run neurological tests, such as a CT scan or x-ray.
Treatment
There are three main forms of treatment for cluster headaches, including the following:
- Pain relief medication
- Preventive care
- Surgery
In most instances, cluster headaches can be controlled and sometimes prevented through medication. Over-the-counter medications usually help to make the pain more tolerable during an episode. Since the cause of cluster headaches is a nerve issue, there are often cluster headache specific treatment options that are effective, including oxygen treatment and nasal spray medications.
In many instances cluster headaches can even be prevented by taking certain prescribed medications, although it is far from 100% effective. Medications such as blood pressure, antidepressant and steroid medications are often effective at preventing cluster headaches. However, be sure to discuss preventive medications with your doctor before beginning treatment.
In the event less invasive treatment and prevention measures do not work to reduce the severity or frequency of cluster headaches, a surgical procedure to disable the trigeminal nerve may be necessary, although the surgery can carry significant risks.
When to see a doctor
It is important to see a doctor anytime cluster headaches are believed to exist for an accurate diagnosis and a long-term treatment plan.
While the symptoms of an episode of a cluster headache can be treated with holistic measures, it most often requires medical assistance and prescribed medication to control cluster headaches in the most effective and efficient manner possible.
Any time a single episode of a cluster headache becomes very severe to the point where the pain or pressure caused by the headache is nearly intolerable it is important to visit a doctor for prompt treatment and to ensure nothing more is wrong.
3. Migraine Headaches


There are two different types of migraine headaches, which are migraines with aura and migraines without aura. An aura is a brief moment in time before a migraine occurs that signals a migraine is right around the corner.
Migraine headaches are typically fairly severe, and the more serious headaches result in a need to visit the emergency room to relieve the discomfort that occurs.
Signs and symptoms
Many of the symptoms of a migraine are similar to more traditional forms of head pain, although there are many additional symptoms that often come along with a migraine that are not present with tension headaches or cluster headaches.
Here are the most common signs and symptoms of a migraine headache:
- Severe head pain
- Sensitivity to light
- Nausea and vomiting
The most obvious symptom of a migraine headache is severe pain on one side of the head, although it is possible to experience pain on both sides of the head. Migraine head pain often feels like a throbbing, sharp pain that causes many to alter or discontinue their daily routine.
Along with the head pain, it is not uncommon for those who suffer from a migraine to experience extreme sensitivity to light and may even not be able to see as clearly during an episode.
In severe instances – although it is not extremely rare – those with migraines may experience nausea and vomiting during a migraine.
Causes
The exact reason as to why individuals experience migraines is difficult to determine. However, there are certain signs and indications that suggest a migraine may develop, which are:
- Emotional stress
- Alcohol use
- Hormonal changes
In many instances, migraines can be completely unpredictable, and the sufferer may not have done anything to directly provoke a migraine. However, by avoiding these three common causes of a migraine episode, individuals who suffer from chronic migraines can lower their chance of an episode.
Perhaps the most prominent trigger of a migraine is emotional anxiety, such as too much stress at work or social anxieties. Also, those who drink alcohol daily are at greater risk of experiencing a migraine.
While it is impossible to prevent, hormonal changes also put individuals at greater risk of a migraine, which means more caution should be taken to prevent a migraine when experiencing hormonal changes.
Diagnosis
Since diagnosing a headache from a migraine can be difficult, it is important to visit the doctor anytime head pain becomes severe, especially if the head pain results in nausea, vomiting or sensitivity to light.
To diagnose a migraine from other forms of head pain, the doctor is likely to rely heavily on medical history, family medical history and an examination of symptoms. However, in some cases neurological testing, such as a CT scan or x-ray may be in order as well.
Once diagnosed, treating and preventing future migraine attacks is much easier to do.
Treatment
Fortunately, there are ways to prevent a migraine attack from occurring in the first place, or at least greatly reduce the frequency as to which they occur.
In order to best prevent a migraine, it is important to reduce as much stress as possible while at work and at home, ensure a proper diet is in place and receive plenty of rest. Also, certain medications such as antidepressants may help reduce the chance of suffering from a migraine attack.
However, even when the proper preventive measures are taken there is still a chance of a migraine attack. When a migraine occurs, there are certain treatment that can be administered to deal with the symptoms in an effective and efficient manner. First and foremost, taking over-the-counter medications such as Ibuprofen can help treat the pain.
Rest and a proper diet during a migraine attack are also important for recovery. Using an eye mask is a great way to receive rest during a migraine.
When to see a doctor
The severity of a migraine headache has a fairly wide range. While some may only experience minor pain and do not experience migraines frequently, others may experience severe, frequent migraine headaches that can cause them to severely alter their daily routine.
In the event migraines begin to change the way you live your life on a daily basis – which can affect your productivity while at work or school – it is important to visit a doctor for diagnosis and long-term treatment.
Also, anytime other serious symptoms exist along with a migraine headache – such as vomiting or impaired vision – it is recommended to visit urgent care or the emergency room for effective and efficient treatment.
4. Sinus Headaches


Sinus headaches are very common in individuals who suffer frequent sinus infections, although they are not as common on their own apart from the development of sinusitis. In most cases, sinus headaches are not very severe, and they can effectively be treated with home remedies and over-the-counter medications.
However, more serious sinus headaches may require medical treatment in order to overcome, especially if the sinus headaches exist alongside other notable sinusitis symptoms.
Signs and symptoms
In many instances a sinus headache displays many of the same symptoms as a tension or migraine headache, including aching head pain that lasts for several hours without relief.
The best way to distinguish a sinus headache from other common types of headaches is to determine whether or not other sinus infection symptoms are present. Here are the most common signs and symptoms that often exist with a sinus headache:
- Cheekbone pain
- Facial swelling
- Nasal congestion
- Ear pain or fullness
- Fever
Most instances of a sinus headache have very obvious signs and symptoms that point towards the headache simply being the result of a sinus infection. By understanding exactly what to look for and how to determine whether or not the head pain is caused by a sinus infection or is the result of something else is important for seeking and administering proper treatment and preventing future headaches.
Causes
As can be expected, the main cause of a sinus headache is a sinus infection, or sinusitis, which results in swelling and inflammation of the nasal cavities.
However, sinus headaches can be associated with a headache that occurs anytime there is swelling and pain in the facial region. It is very common for sinus headaches to exist in individuals with bad allergies. Sinus headaches are often confused with a migraine as they often have many of the same symptoms along with the head pain, including nausea and vomiting in more severe instances.
There are various groups that are at a greater risk of suffering from a sinus headache. Most notably, individuals with a history of sinus headaches are at an increased risk of developing a future sinus headache. Also, those with a family history of sinus headaches may be at an increased risk as well.
Diagnosis
In most cases a simple evaluation of the symptoms and past medical history is enough for a doctor to determine whether or not a sinus headache is the result of a sinus issue or is the result of migraines and other forms of headaches.
While a physical examination along with documentation to other symptoms present and a full history of the patient’s history with headaches is often enough for a diagnosis, the doctor may order a CT scan or an x-ray to verify the exact type of headache the patient suffers from.
After diagnosis, the doctor recommends a treatment and prevention plan to avoid future pain from occurring or worsening in the event one does occur.
Treatment
In many instances the best way to relieve a sinus headache – particularly one that is the result of a sinus infection – is to rest and utilize helpful home remedies, such as nasal spray, using a humidifier and drinking plenty of water.
Many sinus headaches also require the individual to take medication to deal with the current pain and, at times, to treat the underlying cause as well. Simple over-the-counter medications are often enough to relieve pain and pressure caused by sinus headaches.
For sinus headaches that are a symptom of a sinus infection, the best way to relieve the head and facial pain is to treat the underlying cause. If the sinus issues are the result of a bacterial infection, antibiotics can help to fight off the infection in a fast and effective manner, which in return should limit the lifespan and severity of the sinus headache.
Related Article: Holistic Medicine
When to see a doctor
It is important to see a doctor anytime a sinus headache lasts for more than several days, especially if other symptoms of a sinus infection exist along with the sinus headache.
It is also recommended to visit a doctor if the head pain happens on a recurring basis or if the pain is only relieved through over-the-counter pain relief medication.
Most sinus headaches are minor and can be treated with over-the-counter medication and proper home remedies, but any sinus infection that worsens or lingers, causing the individual to miss work or make alteration to their daily routine, should prompt a visit to a doctor for proper diagnosis and treatment.
5. Caffeine Headaches


Many consume a lot of caffeine on a daily basis, and caffeine headaches are much more common than many believe. In many cases, individuals with a caffeine headache may mistake their head pain as another form of headache, when in fact the cause is right in front of them the entire time.
Fortunately, caffeine headaches can easily be treated and even prevented when recognized.
Signs and symptoms
A caffeine headache does not have many signs and symptoms that help distinguish it from other types of headaches, other than the consumption or lack thereof of caffeine.
The most common signs and symptoms of a caffeine headache include:
- Consuming large amounts of caffeine
- Withdrawal from caffeine intake
- Severe head pain in the forehead region
- Unexplained head pain
Caffeine headaches often feel much like a tension headache, with the most prominent symptoms being pain in the forehead region to the scalp, tenderness around the forehead and a slower onset of head pain.
In many cases, those who suffer from a caffeine headache mistake their head pain for another form of headache, especially if they are unfamiliar with what a caffeine headache is.
At the end of the day the most common cause of a caffeine headache is, well, caffeine. By monitoring your caffeine intake, you can not only prevent caffeine headaches, but you can use it to your advantage in headache prevention.
Causes
To fully understand the causes of caffeine headaches, it is important to understand why a caffeine headache occurs. There are various different reasons why a caffeine headache occurs. Here are the most common reasons a caffeine headache might occur:
- Caffeine withdrawal
- A Caffeine overdose
- Caffeine intake changes
- Caffeine allergy
The most common cause of a caffeine headache is a withdrawal from caffeine consumption. After consuming a large amount of caffeine over an extended period of time, the body grows accustomed to the routine and craves the caffeine. When the caffeine is not provided, it can result in a caffeine headache.
Although it is rarer, caffeine headaches can result from too much caffeine consumption at once, which is why relying on caffeine to prevent fatigue is not always a great idea.
In more rare instances, a caffeine headache may be the result of an allergic reaction to caffeine.
Diagnosis
The majority of the time caffeine headaches are fairly easy to diagnose at home. In the event a common pattern of caffeine consumption – such as having a cup of coffee each morning – is broken and a headache results, then the likely cause is a caffeine headache.
In the event a doctor’s visit is necessary due to a potential caffeine headache (see below), the doctor is likely to give a diagnosis after considering the patient’s history with caffeine intake and headaches and rule out more serious causes. On some occasions a CT scan or an x-ray may be required for an accurate diagnosis.
See Also: Headaches Behind the Eyes
Treatment
You can prevent a caffeine headache by ensuring you are not taking in too much caffeine on a daily basis and staying consistent with your caffeine intake. However, managing your caffeine intake is much easier said than done in many instances, and there are occasions when a caffeine headache is hard to prevent.
Fortunately, caffeine headaches are fairly easy to treat. The quickest and easiest way to eliminate a caffeine headache is to simply drink more caffeine, especially if the headache is caused by caffeine withdrawal. Other simply home remedies may help as well, including getting more rest and taking over-the-counter medication.
In the event a doctor’s visit is necessary, the doctor may prescribe prescription pain relief medication and help the patient form a plan for ensuring caffeine withdrawal or consuming too much caffeine does not occur.
When to see a doctor
The majority of the time a caffeine headache does not require medical assistance to properly treat.
However, a caffeine headache that does not go away after twenty-four hours may be the result of a more serious cause other than caffeine, and it may be a good idea to visit the doctor for an accurate diagnosis and treatment. Additionally, any caffeine headache that becomes intolerable may require medical assistance.
It is also important to visit the doctor for caffeine headaches that occur frequently for more than a month. It is unusual for caffeine headaches to occur constantly over an extended period of time, and the headache may be caused by something else if the pain becomes frequent.
6. Exercise Headaches


Exercise headaches are usually not real severe or difficult to treat, although preventing or predicting an exercise headache may be somewhat challenging.
There are two different types of exercise headaches, primary and secondary. Primary exercise headaches are the result of an isolated incident, whereas secondary exercise headaches often are the result of a more serious underlying condition.
Signs and symptoms
There are very few distinguishable signs and symptoms when comparing an exercise headache with a tension headache, although there are some key signs and symptoms that help doctors determine whether a patient is suffering from an exercise headache or another common type of headache.
Here are the most common signs and symptoms of an exercise headache:
- Pain one or both sides of the head
- Pain that results from exercise
- Throbbing, short-term pain
In most instances of a tension, cluster or migraine headache, the pain is isolated to a single area of the head, which is usually on one side of the head or near the forehead. However, an exercise headache often affects both sides of the head simultaneously, and it can cause aching pain that covers a large area.
The most notable difference is that pain from an exercise headache usually happens either during or directly after physical activity, such as walking, jogging or playing a sport.
The pain from an exercise headache is generally the most severe in the first few hours after physical activity, and the pain slowly decreases after the physical event.
Causes
The exact reason people experience exercise headaches is still unclear within the medical community, although it is believed to have something to do with the dilation of blood vessels inside the head, much in the same manner a cluster headache occurs.
However, the correlation between exercise and exercise headaches is quite apparent, and there is little doubt that those who have a history of headaches and are physically active run an increased risk of suffering from an exercise headache during physical activity.
Most commonly, exercise headaches occur during the following physical activities:
- Jogging
- Running
- Swimming
- Weightlifting
- Sport activities
While these activities are the most notable activities that can lead to an exercise headache, they can occur during any physical activity.
Additionally, there may be an increased chance of suffering from an exercise headache when exercising at a high altitude or when the weather is warm.
Diagnosis
An exercise headache is fairly easy to diagnose in most instances. Quite simply, any headache that occurs after physical activity can safely be assumed to be an exercise headache.
In the event medical treatment is needed to treat an exercise headache, the doctor is likely to rule out other common types of headaches – including tension and cluster headaches – before diagnosing the patient with an exercise headache.
The doctor may utilize medical history, family history, lifestyle routines and various neurological tests to determine the exact type of headache.
Treatment
Fortunately, exercise headaches are fairly easy to treat, assuming the exercise headache is a primary exercise headache and there is not a more severe underlying concern causing the head pain.
The best way to treat an exercise headache is by taking over-the-counter medication and receiving an adequate amount of rest. Also, there are certain home remedies that can help relieve pain and pressure caused by an exercise headache quickly, such as wearing an eye mask while resting.
While treatment for an exercise headache is not extensive and has a high success rate, preventing an exercise headache can be much more difficult, especially if the exercise headaches are unpredictable.
If the exercise headaches are fairly predictable, there may be a prescribed medication that can be taken to reduce the chance of an exercise headache, although many exercise headaches are unpredictable and very hard to prevent without altering the amount of physical activity of the individual.
When to see a doctor
Most exercise headaches are not very serious and usually go away within several hours after physical activity stops. However, exercise headaches can grow to be incredibly annoying, especially in individuals who exercise on a daily basis.
If exercise headaches become chronic, it may be a good idea to visit a doctor to try and prevent exercise headaches from occurring during and after physical activity.
Also, if an exercise headache is believed to be the result of a more concerning issue, such as a brain tumor, it is important to visit a doctor as soon as possible.
7. Head Injury Headaches


Head injury headaches vary in severity, and on almost every occasion they require urgent medical care in order to ensure there are no serious concerns that can lead to long term complications.
With prompt care, headaches that are the result of a head injury do not pose any long-term risks, although head injuries that are left untreated or become chronic can pose a serious threat to one’s long term health.
Signs and symptoms
A head injury headache can be much more challenging to diagnose than a normal headache as many of the symptoms affect the brain as opposed to simply the head.
Here are the most common signs and symptoms of a head injury headache:
- Head pain
- Memory issues
- Confusion
- Dizziness
- Nausea
Anytime a blow to the head is suffered and the individual shows signs of a confused mental state, it is likely the individual has suffered a concussion, especially when a head injury headache is present.
In many cases a head injury headache can be confused with an exercise headache in the event the person suffers from headaches when physically active, especially if the blow to the head was not noticed by the person or by others.
In more severe instances of a head injury headache, the person may experience nausea and vomiting, at which point it is important to seek medical assistance.
Causes
There are various causes of a head injury headache. However, most head injury headaches are caused by a blow to the head, such as the following:
- Hit by moving object
- Falling and landing on head
- Car accident and whiplash
Perhaps most commonly head injury headaches occur during physical activity and various contact sports such as football and hockey.
However, a head injury headache can occur anytime there is a blow to the head, including during a fall or as a result of a car accident in which the person experiences whiplash or an impact to head occurs.
By understanding the exact cause of the head injury headache, the individual who suffered the injury and their doctor can best determine how severe the head injury is.
Diagnosis
It is important to receive a professional diagnosis after experiencing a head injury headache, especially if the person shows signs of a confused state of mind.
Upon visiting the doctor, she or he is likely to give the patient a diagnostic test to determine whether or not the patient experienced a concussion. The doctor may also order a CT scan or x-ray in order to determine the full extent of the damage from the injury, including the severity of the head injury headache.
Treatment
It is important to remember that a head injury headache is often a symptom of a more severe issue, and the best way to treat the headache is to treat the underlying cause, especially if the underlying cause is a concussion.
If the underlying cause is a concussion, the best form of treatment is rest and to restrain from further physical activity. It is also important to avoid drugs or alcohol while recovering as well.
For the head injury headache in particular, the doctor may prescribe over-the-counter prescription pain relief medication to be taken in moderation, although too much anti-inflammatory medication may cause difficulties during recovery from a concussion.
Ultimately, the best way to recover from a head injury headache is to rest and practice useful home remedies, such as wearing an eye mask and ensuring there is no exposure to bright lights or loud sounds.
When to see a doctor
It is highly encouraged to see a doctor anytime a head injury occurs, especially a head injury that results in a head injury headache.
If a head injury headache is experienced during physical activity – regardless of how long ago the injury occurred – it is important to stop physical activity immediately.
After the initial visit to the doctor, be sure to visit the doctor again if the head injury headache worsens or lasts for an extended amount of time.
We hope this explanation of the different types of headaches has been useful. As you can see, most can be treated at home, but you should always pay a visit to your doctor if the symptoms become too severe or frequent.